Dr. Sagar Bhargava is a best cataract surgeon in Kolkata
What is cataract & how it forms?
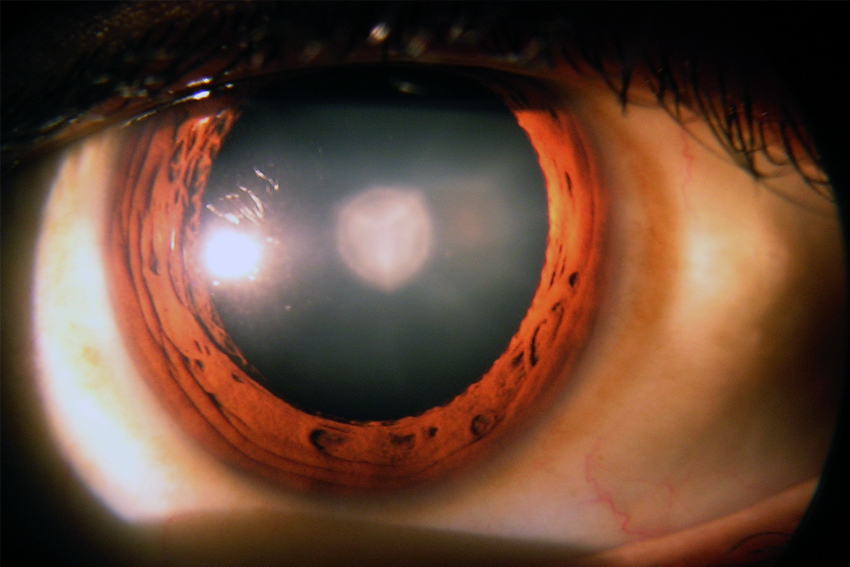
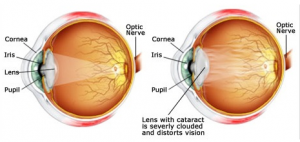 The lens, where cataracts form, is positioned behind the colored part of your eye (iris). The lens focuses light that passes into your eye, producing clear, sharp images on the retina — the light-sensitive membrane on the back inside wall of your eyeball that functions like the film of a camera. A cataract scatters the light as it passes through the lens, preventing a sharply defined image from reaching your retina. As a result, your vision becomes blurred. As you age, the lenses in your eyes become less flexible, less transparent and thicker. Age-related changes cause tissues within the lens to break down and clump together, clouding small areas within the lens. As the cataract continues to develop, the clouding becomes denser and involves a greater part of the lens. Cataracts may develop in only one eye, but they usually develop in both of your eyes. However, the cataracts usually aren’t totally symmetrical, and the cataract in one eye may be more advanced than the other.
The lens, where cataracts form, is positioned behind the colored part of your eye (iris). The lens focuses light that passes into your eye, producing clear, sharp images on the retina — the light-sensitive membrane on the back inside wall of your eyeball that functions like the film of a camera. A cataract scatters the light as it passes through the lens, preventing a sharply defined image from reaching your retina. As a result, your vision becomes blurred. As you age, the lenses in your eyes become less flexible, less transparent and thicker. Age-related changes cause tissues within the lens to break down and clump together, clouding small areas within the lens. As the cataract continues to develop, the clouding becomes denser and involves a greater part of the lens. Cataracts may develop in only one eye, but they usually develop in both of your eyes. However, the cataracts usually aren’t totally symmetrical, and the cataract in one eye may be more advanced than the other.
What are the symptoms?
- Cloudy, blurry, fuzzy, foggy or filmy vision
- A noticeable cloudiness in the pupil
- Increased glare from lights eg: from headlights when driving at night
- A decrease in distance vision but an improvement in near vision.
- Double vision (Diplopia)
- Frequent changes in glass power
- Impairment of colour vision
- Poor vision in sunlight.
Types of cataract
a) Cataracts that affect the center of the lens (nuclear cataracts). A nuclear cataract may at first cause you to become more nearsighted or even experience a temporary improvement in your reading vision. But with time, the lens gradually turns more densely yellow and further clouds your vision.As the cataract slowly progresses, the lens may even turn brown. Advanced yellowing or browning of the lens can lead to difficulty distinguishing between shades of color.b) Cataracts that affect the edges of the lens (cortical cataracts). A cortical cataract begins as whitish, wedge-shaped opacities or streaks on the outer edge of the lens cortex. As it slowly progresses, the streaks extend to the center and interfere with light passing through the center of the lens. People with cortical cataracts often experience problems with glare.c) Cataracts that affect the back of the lens (posterior subcapsular cataracts). A posterior subcapsular cataract starts as a small, opaque area that usually forms near the back of the lens, right in the path of light on its way to the retina. A posterior subcapsular cataract often interferes with your reading vision, reduces your vision in bright light, and causes glare or halos around lights at night.
Some children are born with cataracts. In some cases, the inherited cataract is not significant enough to affect vision. If significant, however, the cataract should be removed in order to avoid vision problems, such as strabismus or amblyopia. Posterior polar cataract — Posterior polar cataracts are characterized by well-demarcated white opacities in the center of the posterior capsule. These opacities often project forward as cylinders penetrating into the posterior lens cortex. Most posterior polar cataracts are asymptomatic or minimally symptomatic. However, over time posterior subcapsular (PSC) opacities may form around the posterior polar opacity. As the PSC progresses, vision may be severely affected. Posterior polar cataracts pose a unique challenge for cataract surgery. The rate of posterior capsular rupture is significantly higher in these cases. The posterior capsule is weakened around the posterior polar opacity and in some cases there may even be a defect in the capsule.
Cataracts can sometimes develop after undergoing eye surgery, such as surgery for glaucoma or retinal surgery. Patients with diabetes sometimes develop cataracts earlier than normal. Also, patients who are taking steroids for an extended period of time may develop cataracts
A traumatic cataract can occur following both blunt and penetrating eye injuries as well as after electrocution, chemical burns, and exposure to radiation.
Techniques of cataract removal
Extracapsular cataract extraction involves the removal of almost the entire natural lens while the elastic lens capsule (posterior capsule) is left intact to allow implantation of an intraocular lens. It involves manual expression of the lens through a large (usually 10–12 mm) incision made in the cornea or sclera. It is very rarely done now a days only indicated for patients with very hard cataracts or other situations in which phacoemulsification is considered to have potential problems
Disadvantages
- Long recovery period 4- 6 weeks
- Stitches are required
- Need injection anasthesia
- Higher risk of intraoperative complications
- Higher incidence of postoperative astigmatism with increased dependence on glasses
- Higher chance of posterior capsular opacification and need for laser capsulotomy
This technique is an evolution of ECCE (see below) where the entire lens is expressed out of the eye through a self-sealing scleral tunnel wound (5-6 mm) . An appropriately constructed scleral tunnel is watertight and does not require suturing. The "small" in the title refers to the wound being relatively smaller than an ECCE, although it is still markedly larger than a phaco wound. The advantage of this technique is low cost.
Disadvantages
- Recovery period is about 3 weeks
- Need injection anesthesia
- Higher postoperative surgical induced astigmatism compare to phacoemulsification
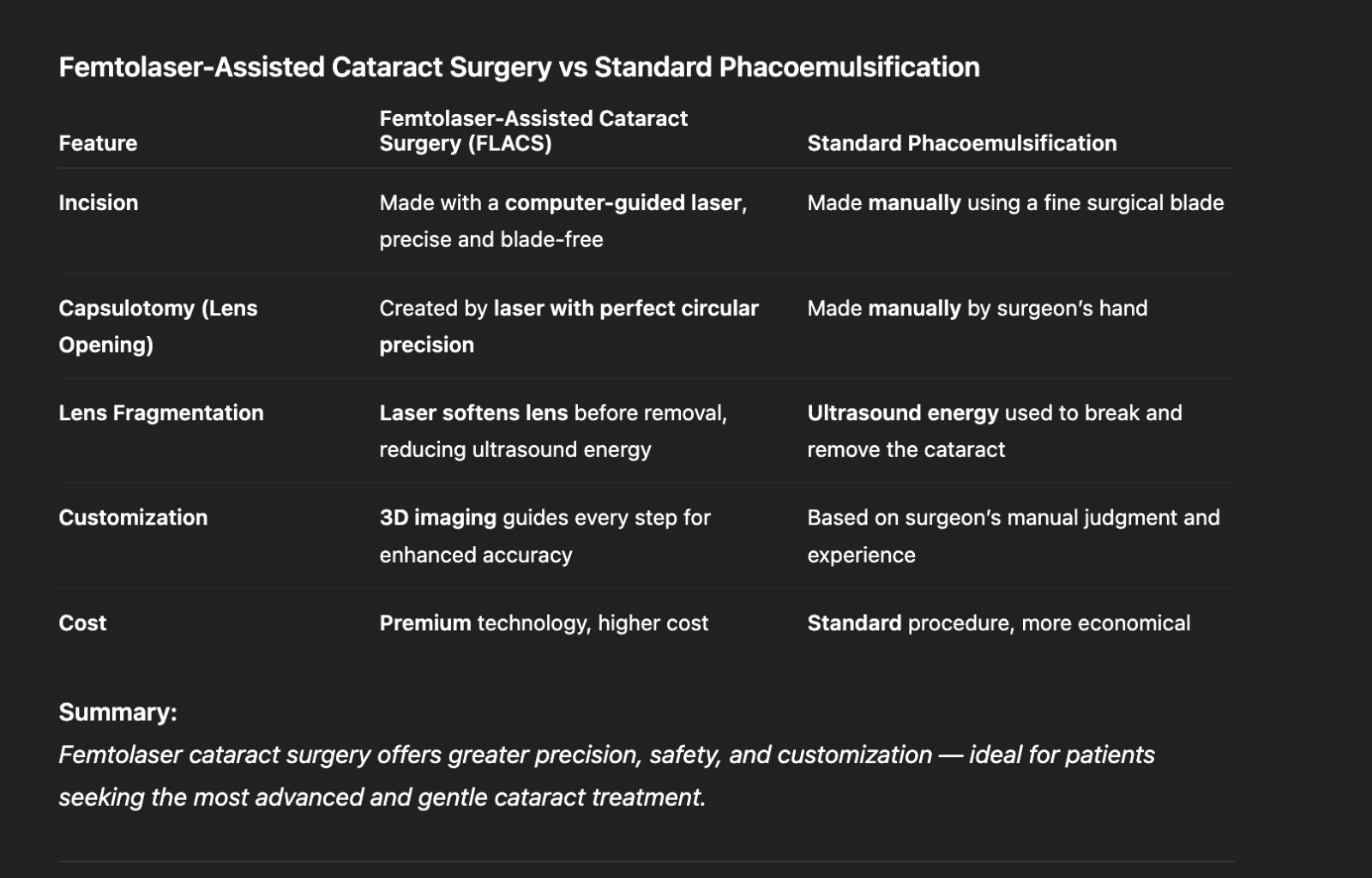
Femtolaser cataract surgery is an advanced, blade-free technique that uses a precise laser to perform key steps of cataract removal with exceptional accuracy. It enhances safety, consistency, and visual outcomes compared to traditional methods, offering a smoother and more customized surgical experience.
A keyhole incision only 2.2- 2.8 mm wide is made on the outside of the eye. A circular opening in the lens capsule exposes the cataract. Next the phaco-emulsifier is inserted. This sophisticated instrument uses high-speed ultrasound waves to break the cataract into tiny pieces which are suctioned out of the eye.
Advantages
- Recovery time is 2 weeks leading to faster visual rehabilitation
- No injection required – done under topical anesthesia
- Minimal postoperative surgical induced astigmatism
Types of IOL
Once you and Dr. Sagar Bhargava have made a decision to undergo cataract extraction, you will be faced with several choices. While cataract surgery has advanced tremendously in the last several years, most of the advances have had to do with the transformation of cataract surgery from a medical procedure to a refractive procedure. Cataract surgery can now allow patients to completely eliminate dependence on glasses for distance, intermediate and near. During your visit, Dr. Sagar Bhargava will discuss the intraocular lens options and vision enhancements are available for your particular case. Dr Sagar Bhargava will help you make the best decision, taking into account your lifestyle demands and hobbies as well and any other limitations.Standard Monofocal IOLsThe standard monofocal IOL has been available for many years. It is also a good choice for those who are happy with wearing glasses after surgery. Although the standard monofocal IOL may reduce a patient's need for glasses, it is designed to replace the cataractous crystalline lens once it has been removed. The patient may expect improved distance vision with minimum correction or without glasses . For near vision patient will need corrective glasses. They are of 2 types based on the design.

The central and peripheral portion are of the same material.

Then central and peripheral portion are of different material . Advantage of this lens is that it can be used in patient who develops a complication like posterior capsular rent.


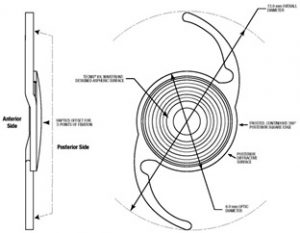
Traditional IOLs are spherical which means the front surface of the the lens is uniformly curved. Aspheric IOLs are slightly flatter in the periphery and designed to provide better contrast sensitivity such as the whereas aspheric intraocular lenses are slightly flatter at the edges to provide better contrast sensitivity. This allows images in a similar color to their background to be more clearly defined.


Toric IOLs are best for patients with significant astigmatism who desire less dependency on glasses.Because they also correct patients' astigmatism, toric IOLs will allow improved distance vision without glasses.
The weakness that toric IOLs share with standard monofocal IOLs is that they are monofocal, allowing either distance vision or reading vision, but not both distance and reading without glasses (unless monovision is employed). Toric IOLs work best with symmetric astigmatism, but they do not correct irregular astigmatism from corneal scarring or other corneal abnormalities. One possible weakness of toric IOLs is that the orientation of the IOL within the eye is critical to addressing the astigmatism. If the lens is not oriented in-line with the astigmatism, the toric IOL may not correct as much astigmatism as it should, and it may even add to the preexisting astigmatism.
EDOF lenses are advanced intraocular lenses that provide clear vision across a wider range — from far to intermediate — reducing dependence on glasses after cataract surgery. They offer smooth, natural vision for daily activities like driving, computer use, and watching TV, with fewer halos and glare than traditional multifocal lenses.

Trifocal lenses are premium intraocular lenses designed to give clear vision at all three distances — near, intermediate, and far — minimizing the need for glasses after cataract surgery. They help patients read, use digital devices, and see distant objects with equal clarity, offering a truly spectacle-free lifestyle for most daily activities.

These are the latest generation of IOL where patients with more than 0.75 diopter preexisting astigmatism can be treated with these lenses to get good unaided distance and near vision
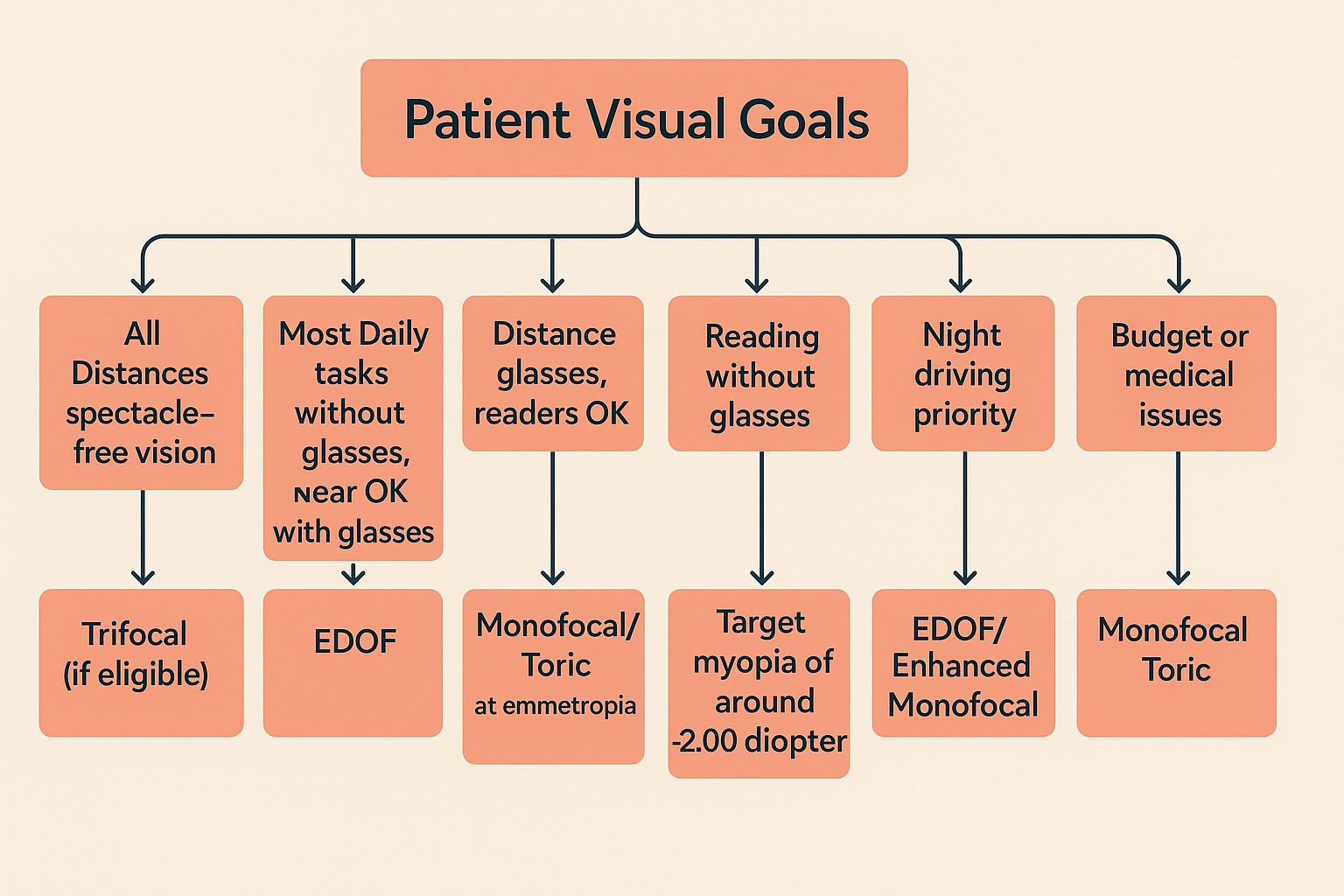
IOL Decision Making
Choosing an IOL is a difficult decision for any patient. The following flow chart is a simplified way of approaching about the question of which lens to implant.