Are Blue Light-Blocking Glasses Worth Itin 2025? Blue light-blocking glasses have become extremely popular — marketed as essential for anyone spending long hours on computers, mobiles, or tablets. Ads promise protection from eye strain, headaches, sleep issues, and even long-term eye diseases. But does science actually support these claims? As an ophthalmologist, here is the latest evidence-based update (2024–25). What Exactly Is Blue Light? Blue light (400–490 nm) is part of visible light — not inherently harmful. Digital screens emit only a tiny fraction of the blue light we get naturally from sunlight. In fact, sunlight gives 100–1000 times more blue light than screens. Is Blue Light From Screens Damaging to the Eyes?Answer: NO No evidence of retinal damage Large studies consistently show: Computer screens emit no UVA or UVB radiation (the harmful spectrum). Screen-emitted blue light is too low in intensity to cause retinal damage in humans. No link to macular degeneration, cataract progression, or blindness. Latest reviews (2023–2024): Ophthalmic & Physiological Optics (2023): “No measurable retinal damage from digital-device light exposure.” Cochrane Review 2023: “No evidence that blue-blocking lenses protect the eye.” Conclusion: Blue light does not harm the retina. Do Blue Light Glasses Reduce Digital Eye Strain? Answer: Also NO Digital eye strain is real — but it comes from behavior, not blue light. Common causes: Reduced blinking → dryness Prolonged focusing → accommodative fatigue Poor posture, glare, improper screen distance Cochrane Review 2023 (17 trials, 619 participants): ➡ Blue-blocking glasses did NOT reduce eye strain, headaches, or dryness compared to normal lenses. American Academy of Ophthalmology (AAO): ➡ Does not recommend blue light-blocking glasses. So, buying expensive “computer glasses” for strain is unnecessary. Does Blue Light Affect Sleep?Answer: YES, but not the eye This is the only area with real evidence. Blue light in the evening can: Suppress melatonin Delay sleep onset Affect circadian rhythm But the source is behavioral, not ocular damage. Best solutions: Avoid screens 2–3 hours before bedtime Use “Night Mode / Dark Mode” Use warm-toned lighting in the evening Blue-blocking glasses may help a bit with sleep only if worn at night, but this is a lifestyle choice—not an eye-care necessity. Should Children Use Blue Light Glasses? Answer: NO Kids using screens for online learning or gaming do not need blue-filter glasses. More important: Frequent breaks Outdoor time (reduces myopia risk) Proper posture Limiting screen time before bed No evidence suggests blue light poses any eye-health risk to children. What Actually Helps Reduce Digital Eye Strain? (Evidence-Based) Follow the 20-20-20 RuleEvery 20 minutes, look at something 20 feet away for 20 seconds. Blink more oftenPurposefully blink to avoid dryness during long screen time. Use artificial tearsPreservative-free lubricating drops reduce dryness significantly. Correct your ergonomics Keep screen an arm’s length (25 inches) away Position slightly below eye level Reduce glare & increase contrast Use good ambient lightingAvoid using screens in dark rooms. For contact lens usersSwitch to glasses during long screen days. So… Are Blue Light-Blocking Glasses Worth It? Short answer: ❌ No — not for eye protection or strain.Long answer: Claim True? Evidence Prevent eye strain No Not supported in any RCT Protect retina from damage No Screens don’t cause retinal damage Prevent headaches No No proven benefit Improve sleep if used at night Maybe Mild effect on circadian rhythm 📞 Book Your Consultation Dr. Sagar Bhargava, MS, FRCSCataract, Glaucoma & Refractive Surgeon – KolkataCall / WhatsApp: +91-9874176663
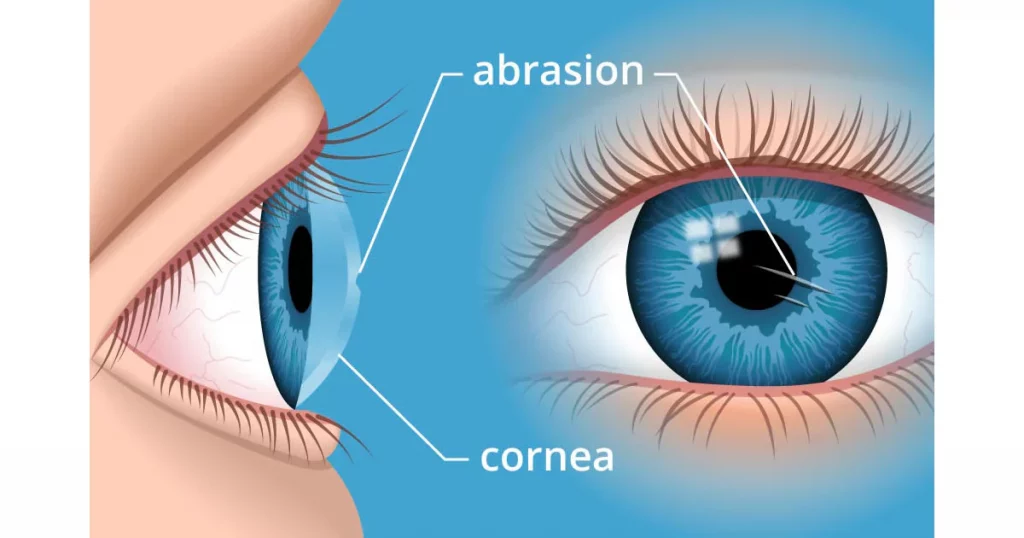
Corneal Abrasion (Scratched Cornea)
Corneal Abrasion (Scratched Cornea) Understanding Symptoms, Causes & Treatment A corneal abrasion is a small scratch on the cornea — the clear, front “window” of your eye. Because this surface has many nerve endings, even a tiny scratch can cause severe discomfort. Common Causes Corneal abrasions can happen due to everyday accidents, such as: Fingernail or object injury (hairbrush, tree branch, makeup applicator) Dust, grit, or foreign particles getting trapped under the eyelid Impact injuries, like walking into something Contact lens mishaps during insertion or removal Symptoms You may experience one or more of the following: Sharp eye pain Redness and excessive watering Light sensitivity (photophobia) Blurred or hazy vision Feeling like something is stuck in the eye Symptoms usually improve within 24–48 hours with proper care. Diagnosis & Treatment During an eye examination, your eye doctor will: Check for foreign bodies Assess the size and depth of the abrasion Use anaesthetic drops temporarily for comfort (not for home use) Typical Treatment Includes: Antibiotic eye drops or ointment to prevent infection Lubricating drops for comfort A protective eye pad may be advised for short-term relief Oral painkillers if needed Home Care & Recovery Tips To help your eye heal quickly and safely: Take recommended pain relievers (e.g., paracetamol) Wear sunglasses to ease light sensitivity Avoid rubbing or touching your eyes Stop contact lens wear until fully healed and cleared by your eye specialist Apply drops/ointment correctly: Wash hands Pull lower eyelid to form a pocket Instill medication Blink gently Most corneal abrasions heal well within a couple of days. Recurrent Corneal Erosion In some cases, weeks or months after healing, you may wake up with sudden pain similar to the original injury. This is called Recurrent Corneal Erosion (RCE). What to do: Seek medical attention Treatment may include night-time lubricating ointments to improve healing When to Contact an Eye Specialist Immediately Seek urgent care if: Pain or redness worsens Vision becomes more blurred The eyelids become swollen Symptoms persist beyond 48 hours
Dry Eye Disease (DED)
Dry Eye Disease (DED) What is Dry Eye? Dry eye is a common condition in which your eyes do not produce enough tears, or the quality of tears is poor. As a result, the surface of your eyes becomes dry, leading to discomfort, redness, and sometimes blurred vision.Healthy tears are essential for clear vision and eye comfort — they keep the surface of the eye smooth and protect it from dust, infection, and irritation. Common Symptoms Burning, stinging, or gritty sensation (like sand in the eyes) Redness and watering Blurred or fluctuating vision Sensitivity to light Eye fatigue, especially with prolonged screen use or reading Difficulty wearing contact lenses Causes Dry eye can result from one or more of the following:Decreased tear production: due to age, certain medications (antihistamines, antidepressants), autoimmune diseases (like rheumatoid arthritis or Sjögren’s syndrome).Increased tear evaporation: caused by meibomian gland dysfunction (oil gland blockage), prolonged screen time, air-conditioned or windy environments.Poor tear quality: when the balance of water, oil, and mucus in tears is disturbed.Diagnosis: A detailed eye examination helps determine the type and severity of dry eye. Tests like tear film breakup time, Schirmer’s test, and meibography may be performed to assess tear quantity and gland health.Treatment:Treatment is tailored to the underlying cause and severity: Artificial tears and lubricating eye drops Warm compresses and lid hygiene to improve oil gland function Prescription medications (anti-inflammatory drops) when needed Lifestyle changes: blink regularly during screen use, stay hydrated, use humidifiers, and avoid direct air flow to the eyes. Prognosis: With proper diagnosis and regular care, most patients experience significant relief and improved vision comfort. Early treatment prevents progression and protects long-term eye health.
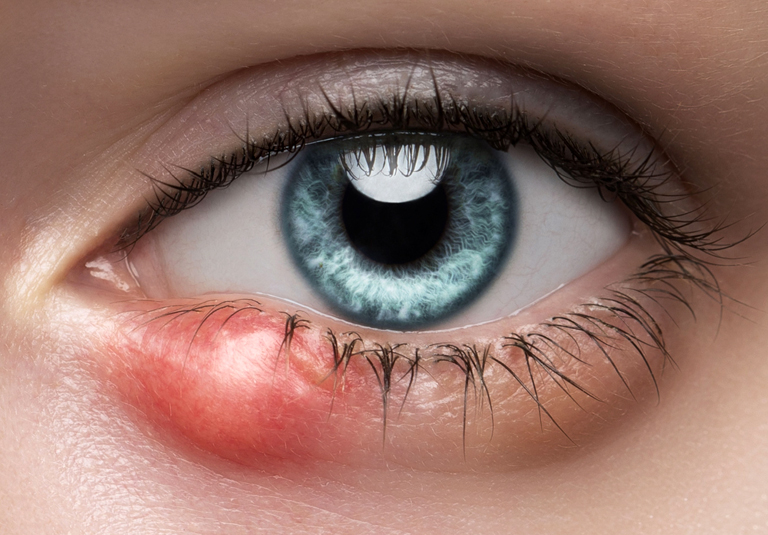
Chalazion (Eyelid Cyst)
Chalazion (Eyelid Cyst) 1. What is a Chalazion? A chalazion is a harmless lump or cyst that develops when an oil gland (meibomian gland) in the eyelid becomes blocked.These glands normally produce oil that helps keep the eyes moist. When blocked, the oil builds up, forming a painless swelling in the eyelid. Usually appears as a small, smooth lump inside the upper or lower eyelid May be red or slightly tender in the beginning Often settles on its own within a few weeks Not contagious and does not affect eyesight A common underlying cause is blepharitis (inflammation of the eyelid margins). 2. Symptoms Small lump or swelling on the eyelid Mild tenderness or irritation at first (usually settles) Sometimes redness of the surrounding skin Discharge may occur if the cyst drains Vision is typically unaffected 👉 In some cases, the lump may remain for several weeks or months as a painless cyst. 🌿 Causes and Risk Factors Blockage of oil (meibomian) glands in the eyelid Chronic blepharitis Rosacea – a skin condition that can affect the eyelids Occasionally after viral conjunctivitis More common in those with oily skin or recurring eyelid inflammation 3. Treatment at Home Most chalazions heal without medical treatment. You can help it resolve faster with the following: 🌡 Warm Compress *Dip a clean cloth in warm (not hot) water*Hold it gently against your closed eyelid for 2–3 minutes*Repeat 3–4 times a day to soften the blockage 💆 Lid Massage After using the warm compress, gently massage the eyelid:For upper lid → massage downwards toward the lashesFor lower lid → massage upwards toward the lashesThis helps the oil drain naturally 🚫 Do Not Squeeze or pop the lumpUse eye makeup or contact lenses until the lump has healedTouch the eyelid frequentlyIf the chalazion drains spontaneously, keep the area clean with cooled boiled water. 💊 Medications Your doctor may recommend: Antibiotic ointment or drops if there is associated redness or infectionPain relief (Paracetamol/Ibuprofen) for mild discomfortOral antibiotics only if infection spreads to the surrounding skin 🔪 When Surgery is Needed If the chalazion: Persists beyond several weeks despite home treatmentIs large, recurrent, or cosmetically concerningThen a minor surgical procedure may be advised. The Procedure Performed under local anaestheticA small incision is made on the inner surface of the eyelidThe cyst contents are gently drainedAn antibiotic ointment and an eye pad are appliedYou can go home the same day Recovery Mild swelling or bruising is common for a few daysKeep the pad for 4–6 hours, then clean gentlyApply prescribed ointment as directedYou may resume work the next day 🔍 Biopsy (Rarely Needed)If chalazions recur frequently or do not heal as expected, your surgeon may take a small biopsy to rule out other rare eyelid conditions. 👦 Chalazion in ChildrenCommon and usually harmlessMost resolve naturally with warm compressesSurgery is rarely requiredSeek advice if the child’s eye becomes red, swollen, or painful, or if vision becomes blurry 4. ⚖ Chalazion vs. Stye Feature Chalazion Stye Cause Blocked oil gland Bacterial infection at lash root Pain Usually painless Usually painful and tender Appearance Smooth, firm lump Red, pus-filled bump Treatment Warm compress, sometimes drainage Antibiotics, warm compress 5. 🩺 When to Seek Medical Advice Contact your eye specialist if: The lump becomes painful, red, or swollen Vision is blurred or there’s discharge The cyst does not improve after 2–3 weeks The problem keeps coming back
Conjunctivitis (Pink Eye)
Conjunctivitis (Pink Eye) 1. What is Conjunctivitis? The conjunctiva is the thin, transparent membrane that covers the white part of your eye and lines the inside of your eyelids.Conjunctivitis simply means inflammation of this membrane, which makes the eyes look red and feel irritated. 2. Types and Causes Conjunctivitis can occur due to: Infection – caused by bacteria or viruses (commonly cold or flu viruses) → Infective Conjunctivitis Allergy – due to reaction to dust, pollen, pet dander or other allergens → Allergic Conjunctivitis 3. Symptoms Depending on the cause, symptoms may vary but can include: Redness and swelling of the white part of the eye and eyelids Itching, burning or gritty sensation Watering or sticky discharge Blurred vision (from discharge or tears) Eyelids stuck together on waking Sensitivity to light Sometimes associated cold, sore throat, or fever (in viral cases) 4. Types of Conjunctivitis Good eyelid care is the most important part of treatment.This should be done twice a day, even when your eyes feel comfortable, to prevent recurrence. Viral ConjunctivitisUsually starts in one eye and spreads to the other.Causes watery, red eyes.May last 2–3 weeks even with treatment.Occasionally, small white spots can appear on the cornea causing temporary glare or blurring.Usually heals on its own with supportive care. Bacterial ConjunctivitisOften produces sticky yellow discharge.Eyelids may be matted or glued on waking.Usually improves faster (within a few days) with antibiotic drops or ointment. Allergic ConjunctivitisTriggered by allergens like dust, grass, or pollen.Causes itchy, watery, red eyes, often in both eyes.May be seasonal (spring/summer) or year-round (dust mite, pets).Not contagious. 5. Preventing Spread (Infective Conjunctivitis) Bacterial and viral types spread easily by: Touching the eyes, then surfaces or other people Sharing towels, pillows, tissues, or eye makeup Sneezing or coughing nearby 6. Prevention Tips: Wash hands frequently Avoid sharing personal items Use separate towels and pillowcases Dispose of tissues immediately after use (Allergic conjunctivitis is not contagious.) 6. Treatment Options For Infective ConjunctivitisMost cases heal naturally in a few days to 2–3 weeks.Antibiotic drops/ointment – helpful only for bacterial infections.Lubricant drops or gel – relieve discomfort but do not shorten duration.Warm compress and lid cleaning – gently remove crusts or discharge.Pain relief – Paracetamol or Ibuprofen can ease irritation or fever.Steroid drops – occasionally prescribed by an ophthalmologist for severe inflammation. For Allergic ConjunctivitisAvoid rubbing your eyes.Use cold compresses to reduce swelling.Lubricant drops for comfort.Anti-allergy (antihistamine/mast-cell stabilizer) eye drops – used daily, often take 1–2 weeks for full effect.Oral antihistamines – can help if symptoms are severe.Steroid eye drops – used only under medical supervision for persistent or severe cases. Contact Lens WearersDo not wear contact lenses during any type of conjunctivitis.Wait until the infection or allergy is completely resolved and lenses have been properly cleaned or replaced. Possible ComplicationsRarely, viral conjunctivitis may cause temporary corneal inflammation, leading to glare or blurred vision.This usually resolves with time and appropriate treatment. When to Seek Medical Advice See your eye specialist if: Symptoms persist beyond 1–2 weeksYou experience pain, light sensitivity, or reduced visionYou have recurrent or severe episodes of allergic conjunctivitis
Blepharitis / Meibomitis (Eyelid Inflammation)
Blepharitis / Meibomitis (Eyelid Inflammation) Blepharitis / Meibomitis is a common, long-term inflammation of the eyelid margins. The rims of the eyelids become red, irritated, and sometimes swollen. It can affect people of any age but is more common in young children and adults over 50.It is not contagious — you cannot catch it from someone else. 1. Symptoms of Blepharitis / Meibomitis his condition often comes and goes, with symptoms flaring up at times and improving later.Common symptoms include: Red, sore, or swollen eyelids Burning, stinging, or gritty sensation in the eyes Itching around the eyes or eyelids Crusts or flakes at the base of the eyelashes Eyelids sticking together on waking up Red or watery eyes Increased blinking or sensitivity to light Sometimes, Blepharitis / Meibomitis can lead to dry eyes or small eyelid swellings (chalazions).When symptoms are active, try to avoid contact lenses and eye makeup until the lids settle. 2. Why Does Blepharitis / Meibomitis Happen? Each eyelid has tiny oil glands that keep your eyes comfortable. In Blepharitis / Meibomitis, these glands can become blocked or inflamed, leading to irritation.It can occur more often in people with skin conditions like eczema, acne, or rosacea, or in those prone to allergies such as asthma.Some people may also be sensitive to bacteria that naturally live on the skin. 3. Treatment and Care Blepharitis / Meibomitis is usually chronic (long-term) and tends to recur. There is no complete cure, but with regular care, it can be controlled very well. The mainstay of treatment is daily eyelid hygiene to keep the glands clear and healthy.If dryness is present, lubricating eye drops (artificial tears) can help. For more severe cases, your doctor may prescribe: Antibiotic ointments or drops for the eyelids Oral antibiotics for a few weeks, especially if rosacea is present Steroid eye drops (short term only) if inflammation is significant 4. Daily Eyelid Hygiene Routine Good eyelid care is the most important part of treatment.This should be done twice a day, even when your eyes feel comfortable, to prevent recurrence. Step 1: Warm Compress (3 minutes)Use a clean, warm flannel or a microwavable eye bag. Hold it gently on closed eyelids for about 3 minutes.This softens the oil in the glands. Be careful not to make it too hot. Step 2: Gentle Lid MassageImmediately after the warm compress, gently massage your eyelids to help clear the oil from the glands.For the upper lid: look down and gently press or roll your finger toward the lashes.For the lower lid: look up and roll upward toward the lashes. Step 3: Cleaning the Eyelid MarginsMoisten a cotton bud with clean water or use ready-made eyelid wipes.Gently clean along the lash line to remove flakes, crusts, and excess oil.Pull the lid slightly away from the eye if needed to clean behind the lashes. 5. Possible Complications If the oil glands remain blocked, a chalazion (meibomian cyst) may form — a small, round, painless bump on the eyelid.Regular warm compresses can help it resolve.Occasionally, the cyst can become red and tender due to infection.Rarely, untreated Blepharitis / Meibomitis can affect the cornea (the clear front part of the eye), which requires prompt medical care. Summary Blepharitis / Meibomitis is common and manageable with regular care.It is not contagious.Daily lid hygiene is the key to keeping symptoms under control.See your eye doctor if symptoms persist, worsen, or affect your vision.
Humphrey Visual field Analyzer
A Humphrey Visual Field Analyzer (HVF or HFA) is a widely used automated perimetry instrument that measures the full extent of a patient’s visual field, or range of sight.
Our Facilities
Dr Sagar Bhargava is available in Netralayam, Kolkata. The hospital is equipped with state of the art diagnostic and surgical equipment’s.
Lattice Degeneration
Lattice Degeneration What is Lattice Degeneration? Lattice degeneration is a thinning and weakening of the peripheral (outer) retina, the light-sensitive layer at the back of the eye.It looks like fine white lines or patches shaped like a lattice (net-like pattern) on retinal examination. It is a common finding, seen in about 6–10% of the general population, especially in people who are nearsighted (myopic). Why Does It Occur? The exact cause is not fully known, but lattice degeneration is thought to occur because of:Stretching of the retina in myopic (short-sighted) eyes.Reduced blood supply in certain areas of the retina. Does It Affect Vision? Usually no.Lattice degeneration by itself does not cause blurring of vision or pain. Most patients are unaware of it until found during a routine eye check-up or dilated retinal examination. Why Is It Important? In some people, the thinned retina can develop small tears or holes, which may allow fluid to enter underneath and lead to retinal detachment — a serious sight-threatening condition. Warning Symptoms to Watch For Seek urgent eye consultation if you notice: Flashes of light (especially in dim light) New black floaters or cobweb-like spots A curtain-like shadow or loss of part of vision These may indicate a retinal tear or detachment. Treatment No treatment is needed for most cases — only regular monitoring. If small holes or tears are detected, you will need prophylactic laser treatment to seal them and prevent retinal detachment.Patient should ideally do a yearly retinal check-up. Prognosis With regular monitoring and prompt treatment of any tears, the long-term outlook is excellent. Most people with lattice degeneration maintain normal vision throughout life. Remember Regular eye examinations help detect retinal changes early — timely treatment can prevent vision loss.
ICL Surgery in Kolkata – Safety, Benefits, Risks & Complete Guide (2025)
ICL Surgery in Kolkata – Safety, Benefits, Risks & Complete Guide (2025) Hello Reader! Welcome to the official blog page of Dr. Sagar Bhargava, one of the best ophthalmologists in Kolkata and a leading expert in cataract, refractive, and ICL surgery. While LASIK remains popular, many patients have thin corneas, high myopia, or dry eyes — making them unsuitable for LASIK or SMILE. For these individuals, ICL (Implantable Collamer Lens) surgery is one of the safest, most effective alternatives. This guide covers everything you need to know: Safety of ICL Benefits & risks Recovery timeline ICL vs LASIK vs SMILE Astigmatism correction Long-term expectations Table of Contents What is ICL Surgery? Benefits of ICL Surgery Risks of ICL Surgery Is ICL Surgery Safe? How quickly will I see improvement? Potential Side Effects ICL vs LASIK vs SMILE Can ICL correct astigmatism? Long-term problems associated with ICL FAQ Conclusion What is ICL Surgery? ICL surgery involves placing a special Collamer lens inside the eye—between the iris and the natural lens. Unlike LASIK, ICL does not cut or reshape the cornea. ICL is ideal for patients with: Myopia up to –20 diopters Moderate to high astigmatism Thin corneas Dry eye tendency Unsuitability for LASIK/SMILE The lens is invisible, painless, and biocompatible. You cannot feel it, and it stays permanently—but can be removed later if required. Benefits of ICL Surgery 1. Treats very high power Corrects degrees of myopia and astigmatism beyond LASIK limits. 2. Reversible procedure ICL can be removed or exchanged if required—an advantage over LASIK. 3. Preserves corneal strength Because no corneal tissue is removed, long-term corneal stability is excellent. 4. Excellent night vision quality Fewer higher-order aberrations mean: Better night driving Sharper contrast Reduced glare & halos 5. Rapid visual improvement Most patients notice clarity within 24 hours. 6. UV protection The Collamer material naturally blocks UV rays. Dr. Sagar Bhargava uses advanced diagnostics and custom vault calculations to ensure safe and precise outcomes. Risks of ICL Surgery Although highly safe, potential risks include: Infection (extremely rare) Increased intraocular pressure Early cataract development Halos or glare Endothelial cell changes Rotation of toric ICL (correctable) With proper screening and follow-up, these risks remain minimal. Is ICL Surgery Safe? Absolutely. ICL surgery has one of the highest global satisfaction rates among refractive procedures. Safety at Dr. Sagar Bhargava’s Clinic Includes: Detailed pre-operative eye mapping Advanced vault prediction formulas Strict sterile surgical protocols Long-term postoperative monitoring How Quickly Will My Vision Improve After ICL? 📅 Within 24 Hours Significant clarity in most patients. 📅 Days 1–2 Mild irritation, dryness, or slight haziness is normal. 📅 Weeks 1–2 Vision stabilizes further. 📅 Week 4+ Most patients achieve full visual clarity. 📅 1–3 Months Final stabilization. Potential Side Effects Temporary blurry vision Glare or halos Mild dryness Increased IOP (rare) Lens displacement (very rare) ICL vs LASIK vs SMILE ICL vs LASIK ICL vs SMILE Cornea preserved No corneal cutting Reversible Effective for very high prescriptions Better for high powers Reversible Less dryness Fast healing Safer for thin corneas Can ICL Correct Astigmatism? Yes. Toric ICL is specifically designed to correct moderate to high astigmatism (1D–4D). Benefits: Accurate alignment Sharp, stable vision Superior quality for high cylinders Long-Term Issues Associated with ICL Rare but possible: Increased eye pressure Early cataract changes Retinal detachment (mainly in high myopes) Endothelial cell reduction Rotation of toric ICL Regular monitoring keeps these risks extremely low. FAQ 1. Is ICL surgery painful? No — it is performed under topical anesthesia 2. How long does the surgery take? 10–15 minutes per eye. 3. When can I return to work? Most patients can return to work within 1 week. 4. Are ICL results permanent? Yes, but the lens is removable if needed. 5. Who is an ideal candidate? Those with high myopia, astigmatism, dry eyes, or thin corneas. Conclusion ICL surgery is one of the safest and most advanced options for long-term freedom from glasses—especially for patients not suited for LASIK or SMILE. With Dr. Sagar Bhargava’s expertise, every ICL procedure is tailored using cutting-edge diagnostics and precision planning. 📞 Book Your Consultation Dr. Sagar Bhargava, MS, FRCSCataract, Glaucoma & Refractive Surgeon – KolkataCall / WhatsApp: +91-9874176663